For hundreds of years, the privilege of being entrusted with the healing arts was inseparable from the devotion of putting patients first. Physicians travelled great distances to visit the sick and care for patients in their homes. Doctors had to be available at all hours and received whatever remuneration families could offer. Although the physician was certainly held in high esteem, their personal interests were largely secondary to the importance of the patient.
By the mid-20th century, healthcare was developing into a mature system and the caregiver-patient dynamic began to change. The relationship was still paramount, but became more paternalistic and emphasized the importance of the physician’s skill and expertise. It wasn’t until the formation and maturation of large healthcare systems that patients’ considerations became fully decoupled from care delivery.
The resulting rise in patient dissatisfaction and the development of novel technology has now begun to swing the pendulum back. Patients are in a position to establish a preeminent role in their care, a role they held for hundreds of years prior to modern times.
1960-1999: A Physician-Centric World
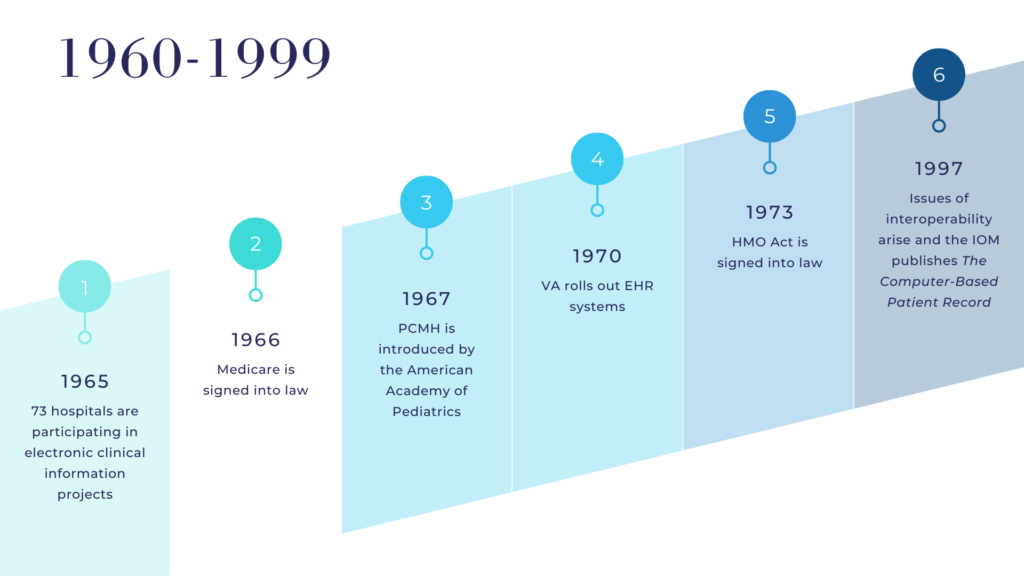
Becoming a physician has long been considered a vocation for the best and brightest rather than merely a path of employment. This notion cemented the physician as an expert atop society’s hierarchical structure for most of the mid to late-20th century.
As a result of their societal status and unique skillset, physicians enjoyed a significant level of independence but lacked consistent income streams. At the same time, wage freezes during the second world war resulted in alternative compensation offerings in the form of health benefits. These prevailing trends led to the first iterations of third party payment services – insurance companies.
The healthcare business model subsequently coalesced into a physician-centric cottage industry; a collection of independent medical practices within local communities that supported a nearby hospital. Patients, for the first time in history, received care on the physician’s terms.
2000-2019: The Rise of Institution-Centric Care
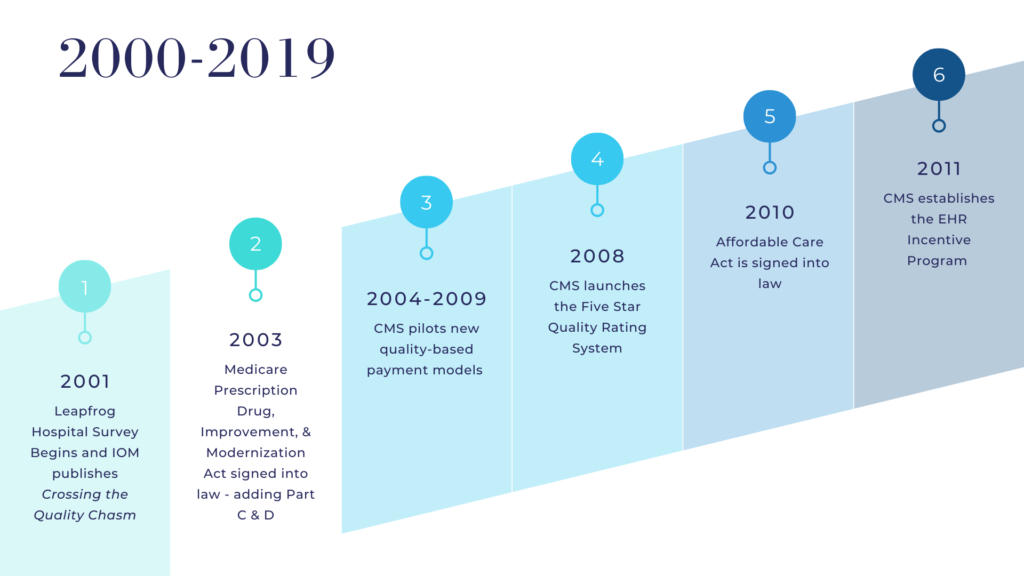
At the turn of the 21st century, several instances of serious medical errors at leading health institutions created ripples throughout the healthcare community. Two sentinel publications, To Err is Human (1999) and Crossing the Quality Chasm (2001), helped quantify the seriousness of the issue and further ignite the movement to improve healthcare quality and safety.
The Quality Movement was the first significant shift that affected both the business and care models. Hospitals had to implement systems, change culture, and improve care to reduce the human variation that led to disparate outcomes. In concert, the payor industry began to incorporate quality and safety outcomes into reimbursement models. The added administrative and fiscal burden pushed physicians to consolidate into large groups or become employed by hospital systems.
This new model contained an inherent flaw – in order to maintain continuity of care and reach quality benchmarks, each patient’s care needed to be confined to one health system. The emphasis on systems as a solution had the unintended impact of distancing individual patient needs from the care they received.
The consequences of an institution-centric model centered on a lack of patient choice and overly bureaucratic workflows that complicated the process of receiving care. A system of layers created considerable frustration while only producing mixed quality and safety results.
2020 & Beyond: The Future is Patient-Centric
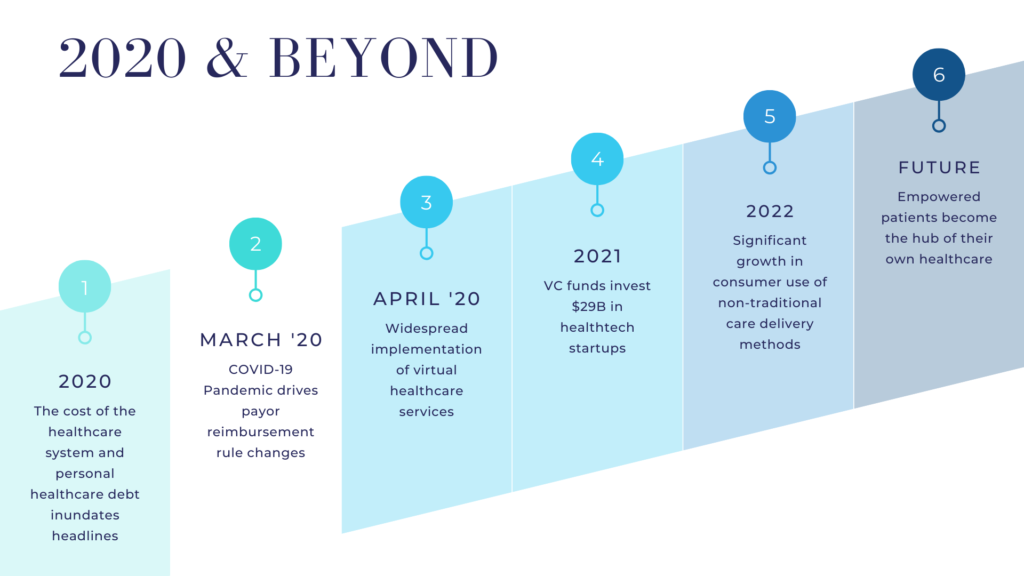
Strict regulations and entrenched incumbents have prevented innovative healthcare startups from disrupting the industry for years. These behemoth organizations governed the ports of entry to care delivery and prevented efforts to reduce friction from reaching scale.
COVID-19 struck the U.S. in March 2020 and created an abrupt need for virtual care delivery. Every healthcare organization across the country adopted some form of telehealth to adapt to the new realities of the pandemic.
After a brief learning curve, patients acclimated to the flexibility and convenience of having the health system meet them where they were, rather than the other way around. A domino effect ensued and propelled nascent startups to engage consumers directly without institutions holding the keys to the gate.
Once patients experienced jurisdiction over their care – how, when, and who they accessed – their expectations were permanently redefined. For large swaths of patients, there was no going back to taking half-days off of work and sitting in a waiting room for a 10 minute face-to-face visit. The industry has begun to recognize that the clinician-patient relationship is a low priority for the consumer. Patients are mobile and willing to switch providers and platforms based on the best value proposition.
Technologies that enable alternative modes of care delivery are forging a path toward patient-managed decentralized healthcare. Patients are empowered and engaging with several new innovations that bring the health system to their fingertips. In 2021, there was a material spike in investments targeting startups in healthtech. Now that the barrier has been broken, the markets are providing solutions to put healthcare back in the patient’s hands, where it truly belongs.
Recommended Resources
Glossary
- PCHM – Patient-Centered Medical Home
- VA – Veterans Affairs
- EHR – Electronic Health Records
- IOM – Institute of Medicine
- HMO – Health Maintenance Organization
- CMS – Centers for Medicare and Medicaid Services
- ACA – Affordable Care Act
- VC – Venture Capital