The present healthcare system is primarily designed to cater to the sick. It does not prioritize the prevention of illness in the healthy. Although this approach may be useful in treating acute ailments, it fails to tackle the underlying reasons for chronic disease. Despite the numerous attempts made by healthcare organizations, quality experts, and CMS to promote preventive care, the outcomes have been abysmal. The lack of progress cannot be blamed on a lack of investment, effort, or academic deliberation.
At the heart of our healthcare system is an engine fueled by incentives to treat episodic acute illness and keep chronic patients stable. People with multiple comorbidities have become an accepted societal norm. With limited resources, the healthy patients are commingled into the same delivery system as the sick and bound to disengage from monitoring their own health. Given the current payment model constraints, it is necessary to align care delivery with the prevailing patient demographics.
Cohorts of Patients
Give me your sick, your healthy, and your Medicare Advantage. Ask any healthcare executive and they’ll tell you that to change the cost/quality equation, you have to first change the payment model. The problem with this approach is the appetite to change the payment model is non-existent – recall the Berkshire Hathaway/Amazon/JP Morgan joint venture attempt? Instead of starting from scratch, we can revolutionize the system from within by grouping patients into cohorts, and tailoring care to the needs of the three populations.
The Sick
Through the two decades of crossing the quality chasm, we have developed a well-established care framework for patients with multiple comorbidities. Comprehensive and detailed metrics that measure all aspects of chronic care management are firmly in place, and providers and hospitals are well-incentivized to meet them. Quality indicators, however, are often reactionary and tend to focus on measuring outcomes after a health event has occurred, rather than preventing it from happening in the first place.
The standardized approach to quality and cost neglects to emphasize the importance of adopting a healthy and goal-oriented lifestyle. The cycle for those with long-term illnesses is never broken.
The Healthy
The reactionary system we have built not only impedes those with persistent health issues from improvement but also accelerates the descent of healthy patients into the sick cohort. This truly forgotten group of healthy people are not yet patients at all. The young, hearty, and seemingly flourishing have been left to fend for themselves with almost zero incentive to engage with the healthcare system unless they absolutely must. By catering to the sick, we have erected a never-ending series of barriers to be a proactive healthy patient.
The Medicare Advantage
A test case for every healthcare executive’s unicorn care model is the cohort of Medicare Advantage patients; a paradox of maximizing risk-based payment while taking a holistic approach to keep patients healthy. While this cohort has grown by 2.7 million1 in 2023, their benefit plans are rooted in a full-risk payment model and require a separate approach to care altogether. The next decade will see one of the most substantial shifts in payer mix that the U.S. has ever experienced. This provides a unique profitability lever for resourcing a health-focused healthcare system.
Healthy as a Priority
What does a health-focused health system look like? Oddly enough, we already have and use many of the tools needed to shift care model priorities. The key lies in successful implementation by: (1)differentiating modes of care delivery based on clinical appropriateness, (2)prioritizing rising-risk health trajectories, (3)creating workflows that maximize productivity and engagement.
The case for healthy as a priority in three charts:
Across the Ages
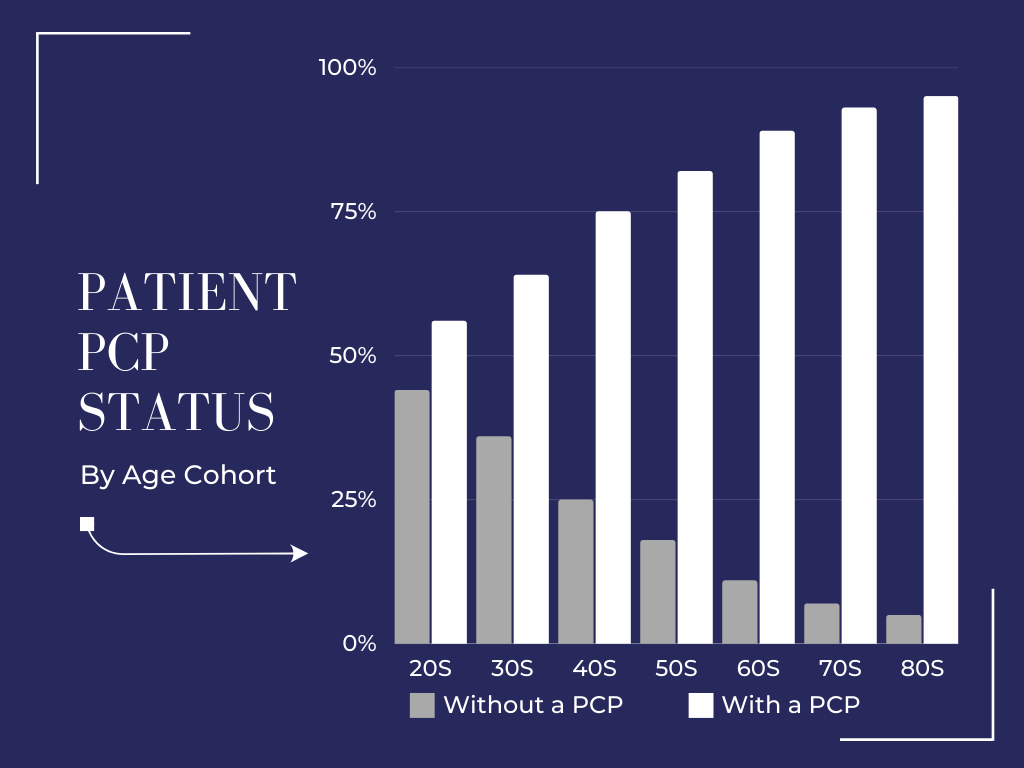
1 in 5 Americans haven’t seen a doctor in at least 5 years2, and more than 100M people in the U.S. don’t have a primary care provider3. The percentage of people accessing preventative care has been on the decline since 2002, and we see the most significant slump in engagement for those in their 30s4. We know that patients who have regular PCP visits are healthier overall, but the younger population is seeking alternate modalities with lower barriers. The system has to meet them where they are.
In Sickness & in Health
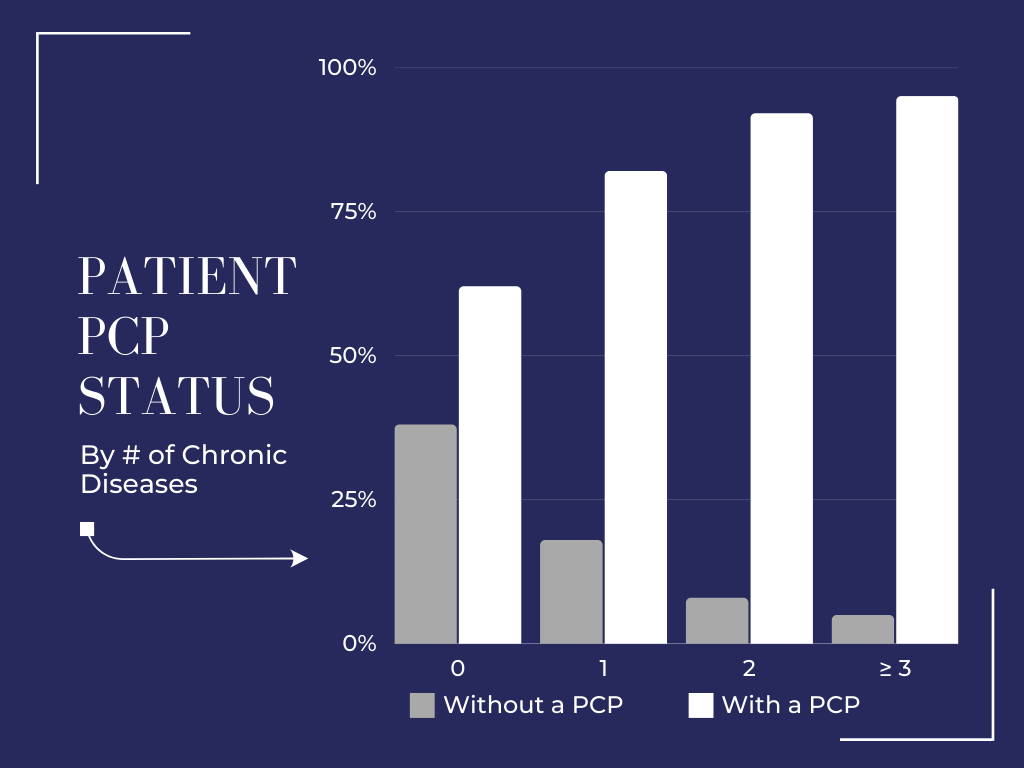
Most healthy people are choosing to engage with the healthcare system on an ad hoc basis or when absolutely necessary. Nationally, 29% of patients who received medical services between 2016 and 2022 did not visit a primary care provider5. Instead of making use of proactive preventative care, patients without chronic conditions are making heavy use of urgent care and ER services.
Provider v. Patient
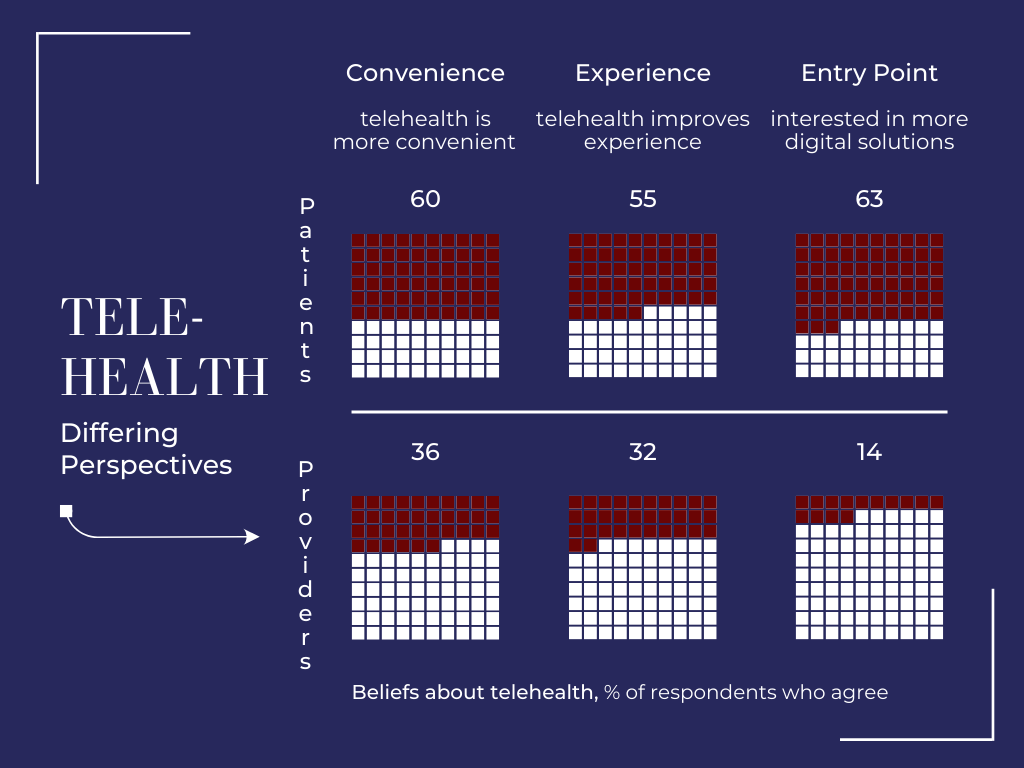
The divergence in the perception of telehealth is a proxy for the persistent expectation gap between how providers want to deliver care and the way patients want to receive it. In 2021, 35% of all consumers reported switching healthcare providers and 1/3 of those switching cited experience/convenience as the reason6. To make telehealth, wearables, and other non-traditional health platforms tenable for clinicians, the operational model must eliminate the duplication of work and enable supportive integration.
Locus of Control
Every year, healthcare administration costs the U.S. $800B with $265B of that outlay going to satisfy unnecessary regulatory/admin tasks7 – that tops what we spend on both cancer and heart disease. This is the result of the entire healthcare sector’s attempt to preserve authority and maintain control.
In 1976, Dr. Russell Roth, President of the American Medical Association, acidly remarked “Passengers who insist on flying the plane are called hijackers” when referring to patients involving themselves in care decisions. My how times have changed. Today, patients have a breadth of resources available at their fingertips – they can read JAMA publications online, monitor their heart rate in real-time, and track fertility on their iPhone. The geographic center of healthcare is making a seismic shift away from providers/systems and towards the patient. An engaged patient is a healthy patient. By involving healthy patients in their care, proactive health-focused models foster greater trust between patients and providers, resulting in informed wellness goals, better adherence to treatment plans, and reduced healthcare costs.
Recommended Resources
- Article – WSJ: Dreaded Medical Paperwork Required by Health Insurers to be Trimmed
- Article – Business Wire: Atrium Health and Best Buy Health Partner to Improve Experience When Receiving Care at Home
- Report – Golub Capital: U.S. Middle Market Growth Continues to Exceed Expectations
- Blog – Windrose Ventures: An Evolution of Healthcare